Analysis: State history of limiting public healthcare contributes to growing risks
Decreased access to Medicaid and Affordable Care Act subsidies will limit options for lower income residents -- and for anyone dependent upon rural hospitals
Mississippi’s Medicaid history epitomizes the enduring ambivalence of state leaders toward federal social programs.
Since the healthcare program’s inception in 1965, state officials have navigated the tension between accepting federal assistance and preserving state autonomy, continually debating the appropriate scope of government intervention in the lives of citizens.
These debates—rooted in fiscal conservatism, administrative control and skepticism of federal oversight—have shaped not only healthcare policy but Mississippi’s broader political culture.
In 2025, Mississippi again occupies a central place in national discussions about healthcare access and the structure of federal support. Recent data from the Urban Institute projects that Mississippi will experience the most severe per-capita effects in the United States if the enhanced premium tax credits under the federal Affordable Care Act expire at the end of the year.
The projected consequences include a $1 billion reduction in total healthcare spending, a 29.1 percent increase in uncompensated care—amounting to approximately $251 million in additional costs to hospitals and providers—and a decline of more than 50 percent in subsidized marketplace enrollment. Adjusted for population, Mississippi would face the sharpest decline in coverage in the nation.
While these figures are tied to current federal policy, they also reflect deeper structural and historical patterns in Mississippi’s healthcare system. The state’s persistent fragility in healthcare delivery has roots in long-standing economic constraints, limited public investment and the gradual dismantling of state-supported medical institutions during the past half-century.
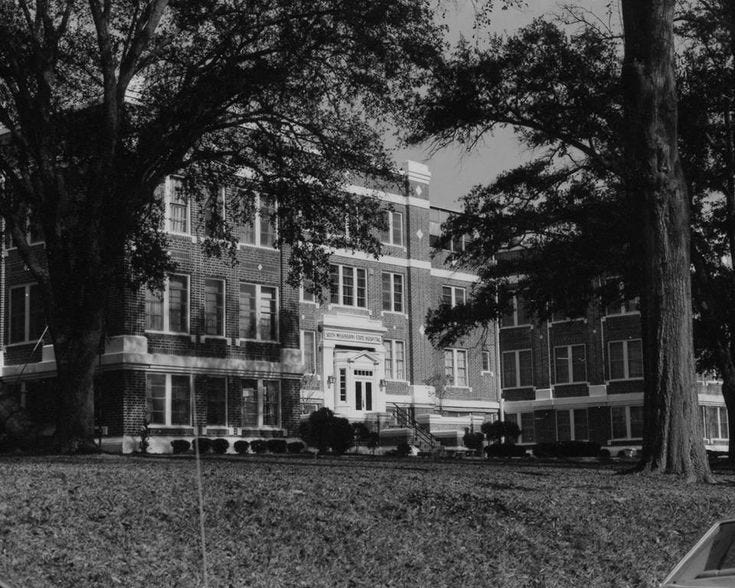
Mississippi’s current circumstances are part of a broader regional trajectory in which southern states reduced or eliminated their public hospital networks in the late 20th century. For much of the century, the region’s charity hospitals formed the backbone of medical care for the uninsured and indigent. Mississippi’s state charity hospitals, operated in Laurel, Vicksburg and Meridian through the University of Mississippi Medical Center, served as the principal institutions of this system.
The state’s ambivalent relationship with federal healthcare programs extends back to the establishment of Medicaid itself. When President Lyndon Johnson established the healthcare program as part of the Great Society, it represented both a landmark expansion of federal social policy and an extension of the civil rights project into the realm of healthcare. Across the South, the new program confronted entrenched systems of racial and economic inequality. In Mississippi, opposition to Medicaid mirrored earlier forms of resistance to desegregation and voting rights enforcement—a defense of “local control” and a rejection of perceived federal intrusion.
State leaders framed their objections in fiscal and ideological terms. Governors and legislators argued that participation in Medicaid would threaten state sovereignty, expand the welfare state and undermine private responsibility. In practice, these objections served to preserve existing racial and class hierarchies. Conservative officials requested repeated delays in implementation, warning that federal health programs would impose unsustainable costs and usher in “socialized medicine.”
On Feb. 4, 1969, Mississippi’s long resistance to federal social programs confronted a decisive turning point. Claude Ramsey, president of the Mississippi AFL-CIO, formally urged Gov. John Bell Williams to implement the federal Medicaid program, marking a rare moment when organized labor became a primary advocate for social welfare expansion in a deeply conservative state. Ramsey’s statement was both pragmatic and political. He argued that Mississippi could finance its share of Medicaid from existing revenue sources, emphasizing that “it is not necessary to increase the tax on gasoline.” This position challenged one of the principal arguments used by state leaders to delay implementation—that the program would require burdensome new taxes and threaten fiscal stability.
The AFL-CIO’s intervention represented a significant pressure campaign. In a state where organized labor had limited influence and social policy had long been filtered through racial and ideological resistance, Ramsey’s appeal reframed the issue as one of administrative feasibility rather than political ideology. By asserting that Medicaid could be established without tax increases, the AFL-CIO effectively dismantled a central justification for delay. The union’s involvement also linked the question of healthcare access to broader struggles over economic justice, signaling the emergence of new coalitions in support of federal social policy.
Supporters proposed funding Medicaid through a reallocation of state resources, including the dissolution of the Mississippi State Sovereignty Commission, the segregationist intelligence agency that had operated for years under the banner of states’ rights. State Rep. Robert Clark, Jr., who died earlier this year, also sought to expand eligibility to welfare recipients who had been excluded under earlier proposals. These efforts provoked fierce resistance from conservative legislators including state Sen. W. B. Alexander of Cleveland, who denounced Medicaid expansion as fiscal recklessness and “government overreach.”
Gov. John Bell Williams eventually called a special legislative session in 1969, bringing these tensions to a head. The debates were protracted and heated. Fiscal conservatives emphasized budgetary restraint, while Medicaid supporters appealed to human need. At one point, Rep. Sterling Seabrook collapsed on the House floor, an episode that seemed emblematic of the session’s intensity. In the end, the Medicaid bill passed the House 79–34 and won Senate approval on Aug. 7, 1969. Mississippi became the second-to-last state to join the program—a late and reluctant participant in the national safety net, achieved only through sustained moral and political pressure.
The 1969 episode established a pattern that would define Mississippi’s welfare politics for decades. Social programs were implemented hesitantly, often under duress, and were subsequently constrained by retrenchment and reform. During the 1990s, welfare restructuring imposed work requirements and time limits that disproportionately harmed Black and poor communities. This pattern of resistance and reluctant accommodation would continue to shape the state’s approach to healthcare policy well into the 21st century.
In 1989, during the administration of Gov. Ray Mabus, Mississippi closed its state charity hospital system as part of a restructuring effort aimed at modernizing healthcare delivery. The closures reflected both fiscal pressures and shifting policy priorities at the national and state levels. Across the U.S., the 1980s had witnessed declining federal social expenditures, the implementation of Medicare’s Diagnosis-Related Group reimbursement system, and increasing emphasis on privatization and cost-efficiency. These developments rendered many public hospitals financially unsustainable.
Mississippi’s decision paralleled trends elsewhere in the South, most notably in Louisiana, where the storied charity hospital system entered a prolonged period of decline. The transition marked a significant shift from centralized, state-supported medical care toward a fragmented arrangement reliant upon private providers, insurance markets and federal subsidies.
The legacy of this regional shift remains evident in Mississippi’s healthcare infrastructure. The absence of a comprehensive public hospital system has left the state dependent upon small community and rural hospitals that now face mounting financial strain, in large measure due to the state’s refusal to expand Medicaid and cuts to the federal program by the Trump administration. Marginally profitable hospitals, which includes most of Mississippi’s rural hospitals, are reliant upon Medicaid reimbursements for their bottom line.
When the Affordable Care Act was enacted in 2010, it sought to address such structural vulnerabilities by further expanding Medicaid and creating subsidized insurance marketplaces. Mississippi lawmakers’ decision not to expand Medicaid eligibility has left a sizable portion of its population in a coverage gap: too poor to afford private insurance but ineligible for Medicaid assistance. In the 21st century, Mississippi’s refusal to expand Medicaid under the Affordable Care Act has perpetuated gaps in coverage, leaving hundreds of thousands without access to care—echoing the same patterns of resistance that delayed the state’s initial entry into the Medicaid program more than four decades earlier.
The temporary enhancement of Affordable Care Act premium tax credits in 2021 reduced this gap, but the scheduled expiration of those subsidies in 2025 threatens to re-expose the underlying weaknesses of the system. As of the mid-2020s, Mississippi reports 23 rural hospitals at immediate risk of closure and approximately $600 million in annual uncompensated care costs. The potential withdrawal of federal support recalls earlier episodes in which fiscal and institutional restructuring placed new burdens on local providers and patients alike.
The contemporary policy debate reflects enduring political patterns. The enhanced ACA tax credits originated in the American Rescue Plan Act of 2021 and were extended under the Inflation Reduction Act of 2022—both passed under Democratic congressional majorities. In Mississippi’s congressional delegation, only Rep. Bennie Thompson supported the legislation; all Republican members opposed it. This partisan division aligns with the state’s history of skepticism toward federal intervention in healthcare and preference for state-level control over social policy.
From Mississippi’s reluctant adoption of Medicaid in 1969 to the closure of the state charity hospital system in 1989 and the contested implementation of the ACA and its subsequent modifications, Mississippi’s healthcare system illustrates the long-term interplay between federal reform, state policy choices and economic constraints. The debates of 2025 thus continue a pattern established over decades—one in which the balance between national support and local autonomy has repeatedly defined the state’s approach to public health and medical access.
In July, Congress passed President Donald Trump’s “One Big Beautiful Bill,” sweeping legislation that reduced federal funding for Medicaid by 12 percent nationwide and imposed new work requirements on adults aged 19 to 64. Proponents justified the measure as promoting fiscal efficiency and personal responsibility, framing the cuts as necessary to eliminate waste and abuse in federal programs.
Mississippi Gov. Tate Reeves, addressing the proposed federal cuts to Medicaid, maintained that Mississippi would be largely insulated from their effects because the state had not expanded coverage under the Affordable Care Act. He cited a 6.5 percent increase in state Medicaid spending—raising the budget to nearly $1 billion—as evidence of sound fiscal management, and argued that new federal restrictions, including work requirements, would “have very little or no impact” on non-expansion states. Reeves’s remarks reflected a continuation of the fiscal reasoning that guided earlier administrations, emphasizing prudence and autonomy over broader social investment.
Yet independent analyses suggest otherwise. The Kaiser Family Foundation estimates that Mississippi could lose between $3 billion and $5 billion in federal Medicaid funding, despite its non-expansion status. The state’s healthcare system—already heavily reliant upon federal dollars—is particularly vulnerable. New restrictions on provider taxes, a key mechanism allowing states to bolster hospital reimbursements, threaten to reduce funding by hundreds of millions of dollars beginning in 2028. Mississippi Hospital Association CEO Richard Roberson has projected that cumulative losses could reach $1 billion during the next decade, imperiling hospitals already strained by low reimbursement rates and high levels of uncompensated care.
The potential impacts extend far beyond budgetary figures. Nearly one-third of Mississippi’s rural hospitals—20 in total—are classified as at immediate risk of closure. Medicaid financed nearly two-thirds of births in the state, the second-highest proportion in the nation, making it central to maternal and infant healthcare. The state’s infant mortality rate has risen sharply enough to trigger a public health emergency. Analysts project that up to 33,000 residents could lose coverage if proposed cuts were enacted.
The 2025 debate has thus revived the same themes that defined Mississippi’s 1969 deliberations: tension between fiscal conservatism and public welfare, between state control and federal partnership, between ideology and pragmatism. The rhetoric of “efficiency” and “self-sufficiency” has persisted, even as the structural conditions of poverty and poor health have endured. As before, the state’s approach to federal healthcare policy illuminates deeper questions about the nature of governance in Mississippi—how responsibility is distributed between state and nation, and how notions of independence and restraint continue to shape public life.
If history offers guidance, it is that meaningful policy change in Mississippi has seldom resulted from executive will alone. In 1969, Medicaid’s adoption followed sustained, cross-sector mobilization. In 2025, similar coalitions—led by the state Legislative Black Caucus, healthcare associations and local advocates—are again pressing for reform.
It is not yet known whether these efforts will yield comparable transformation, but the continuities between past and present suggest that the outcomes of Mississippi’s current Medicaid debates will once again reveal not only fiscal priorities but the moral and political boundaries of the modern state.
Image: Laurel’s now-shuttered Charity Hospital in the 1980s (via Historical Images Collection, Special Collections Department, Mississippi State University; credit: Dr. Lucius Marion Lampton)




I was born and raised in MS and most of my family still lives there. After both my parents died, mom being the last in 2012 I'll never go back to the state for any reason! It makes me sad to see and hear what goes on there but there is no way I can change anything. Until the people understand that the only way out is education then it will always be this way. Fortunately my father thought it important that we get a college education.....I was the first of 10 children to go to college and 2 of us never did. I left the state in 1966 when I married and moved to my husband's home town in VA.